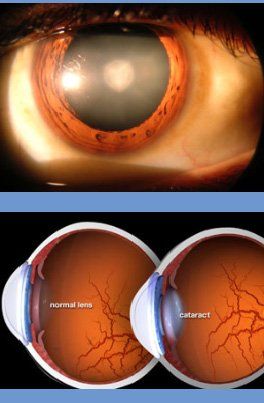
What is Cataract?
- Cataract is the haziness of the crystalline lens of the eye. It causes scattering of light & blurring. It is not a layer that grows on the eye as many think.
- Vision in dim or bright light may get affected. Headlights may cause glare at night. Spectacle power may change frequently. Day to day activities, working with gadgets, using stairs etc., will be increasingly difficult. Reading may improve initially.
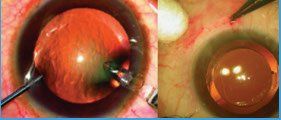
- It is best not to wait for cataract to mature as it can end up in complications. Except in special circumstances, a cataract surgery is performed when you cannot perform your day to day activities adequately and safely due to visual difficulties produced by the cataract. Many professions which demand very good eyesight may need an early surgery. However the natural lens, even with its slight imperfections of an early cataract, would have several advantages over the man made IOLs.
- Cataract does not cause pain, headache, redness or watering. The vision loss in cataract is always slow, and if you ever have rapid or sudden decrease in vision, it should be informed, as you may need specialized investigations to exclude other eye diseases.
- Cataract is common in middle age and in the elderly. It is also caused by drugs, chemicals, injuries, sun, UV light, radiation, electric shocks, malnutrition, diabetes, chronic diarrhea, X- rays, drugs etc. Viral infections during pregnancy, marriage within relatives, Genetic abnormalities etc. can cause cataracts in children.